
Healthy cartilage thanks to bio-ink
What can be done to aid cartilage regeneration in damaged joints? This question is at the heart of the TriggerINK project, which was recently awarded funding from the Werner Siemens Foundation. As a visit to the project team’s lab at DWI – Leibniz Institute for Interactive Materials has made clear: regenerating cartilage takes novel materials, modern technology—and teamwork.
Conventional wisdom has it that the best researchers are loners—solitary introverts who shut themselves away from the world, poring over a problem until the solution reveals itself in a flash of inspiration. And while it’s true that some of the great questions of our time have been solved this way, many research endeavours are simply too complex to be mastered by a single person.
That’s why no less than four research groups are working together in the TriggerINK project at DWI – Leibniz Institute for Interactive Materials. The aim of the large-scale undertaking, which the Werner Siemens Foundation is supporting with 10 million euros over a five-year period starting in 2022, is to develop a visionary method for cartilage regeneration.
The project is led by Laura De Laporte, member of the scientific board at DWI in Aachen and professor of advanced materials and biomedicine at RWTH Aachen University. Also on the team are her RWTH colleagues: Stefan Hecht, DWI scientific director and professor of macromolecular chemistry; Andreas Hermann, DWI deputy scientific director and professor of macromolecular materials and systems; and Matthias Wessling, member of the scientific board at DWI and professor of chemical process engineering. A team of external experts also supports the project in an advisory capacity.

Problem point: the joint
TriggerINK aims to address one of the most common health issues of our time: joint pain. Although its causes are varied, cartilage loss (osteoarthritis) or a damaged meniscus in the knee number among the most frequent complaints. In Germany, one person in five has been diagnosed with osteoarthritis at some point in their life—and the numbers are set to increase as the population ages and obesity continues to rise.
Cartilage and the menisci have important functions: they absorb shock, they distribute the pressure exerted on the knee during movement and they enable bones in a joint to move quickly and smoothly, with minimal friction. However, worn or injured cartilage tissue can’t regrow on its own, and although modern medicine has developed therapies such as cartilage transplantation as well as substances that promote tissue regeneration, these procedures are sometimes prohibitively expensive or their applicability is limited to a small subset of patients. And there’s no guarantee of success.
One of the greatest difficulties in current cartilage regeneration methods is creating the tissue’s structure, explains Laura De Laporte. Cartilage in the knee joint comprises different zones. First, and directly over the bone, it forms a hard layer with a vertical microstructure that new bone stem cells can penetrate only very slowly. The next and main layer, the middle zone, has a rather random cell structure. This is covered by the third zone, a smooth outer layer, whose cells and cell components are horizontally aligned. “Every tissue and every structure in our body has a clearly defined alignment,” says De Laporte. “That’s why it’s imperative in tissue regeneration to steer cell growth in the right direction.”

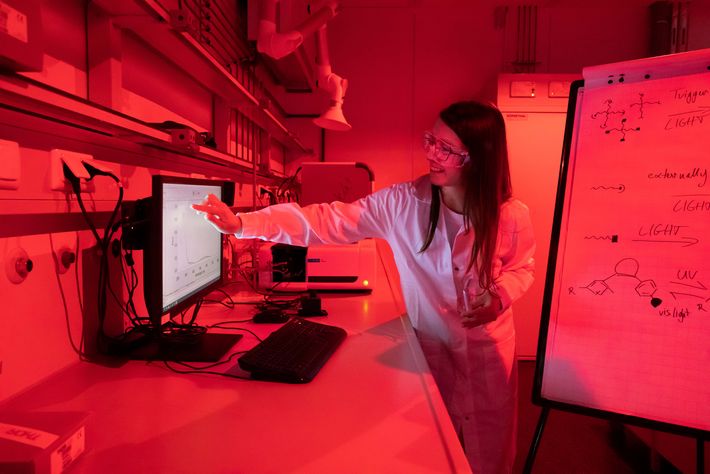
Photoswitch trumps protective cap
Hecht and his team are therefore researching an innovative alternative: molecular photoswitches. This involves synthesising certain molecules that change their form and properties when irradiated with light. The approach has the advantage that no additional protective caps are required. The synthesis of photoswitch molecules is complex, but Stefan Hecht believes he and his team are on the right track. “The system works. After all, improving and accelerating syntheses is the core competency of a chemist,” he says.
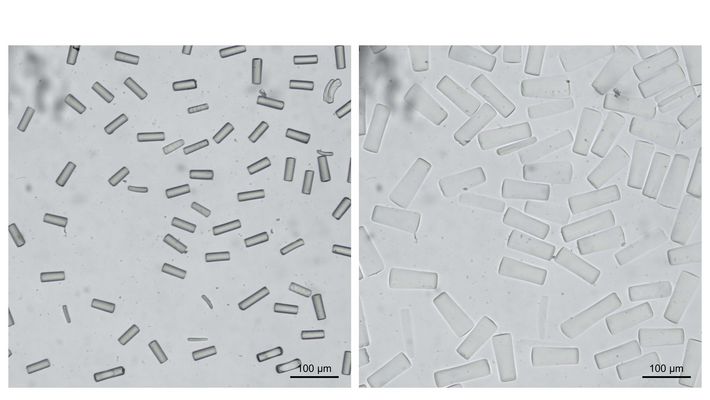
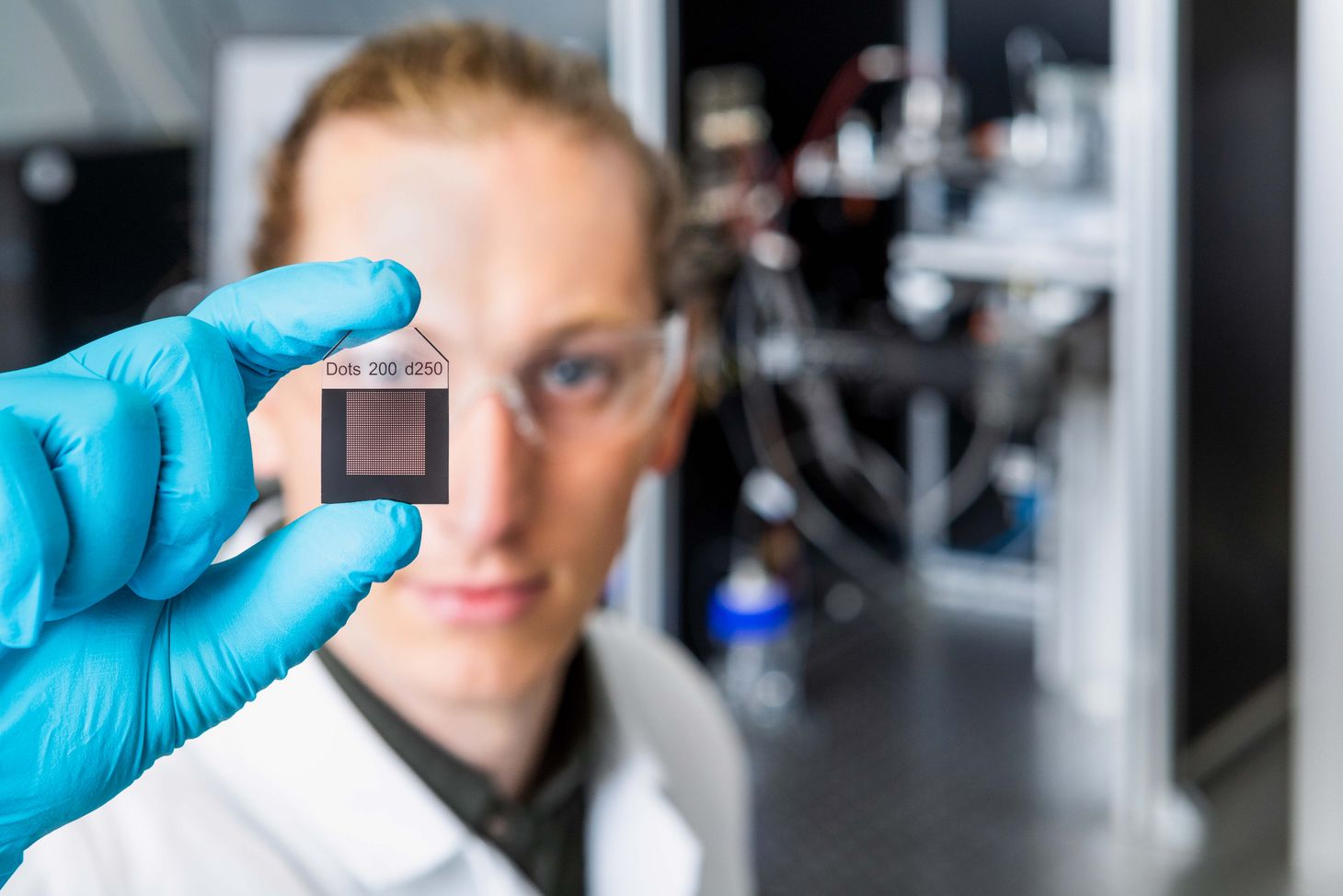
Producing the magnetic rods for the bio-ink is the terrain of Matthias Wessling and his research group. Like the bio-ink itself, the microrods are also made of a hydrogel; they contain magnetic nanoparticles. The rods are produced using a customised machine developed by the process engineers in Wessling’s team. In a method called stop-flow lithography, the polymer flows through fine tubes and is then hardened in specific regions by ultraviolet light.
With the help of templates, the hydrogel can be shaped not only into rods but also an endless variety of other shapes. “We’ve already been able to substantially improve the stop-flow method in the first few months of the project,” says Matthias Wessling. Among other developments, a new production machine is also in the pipeline.
Reactions in the body
The team carefully study the properties of the produced rods and particles; models are used to show how the rods and particles react when, mixed into the bio-ink, they’re introduced into the body using a cannula. Do they gather on a boundary layer? How do the rods and the ink interact? Answering such questions is essential if unintended outcomes are to be avoided. It also demands intense collaboration between the various groups.
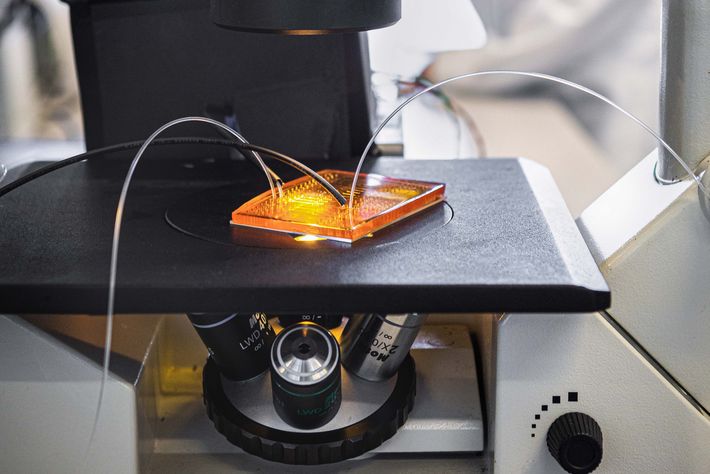
The fruits of these efforts can be admired in another lab. A member of Laura De Laporte’s team prepares a culture dish with bio-ink containing magnetic rods and holds two magnets close to the dish. Viewed under the microscope, it becomes apparent that the rods have all turned in the same direction. The ink is then solidified and a new layer is applied, whose nanorods are facing in a different direction. With this process, the researchers are able to simulate the differently aligned cell layers in different cartilage zones.
Growth on demand
Andreas Hermann and his research group are responsible for the next step in the TriggerINK procedure—using ultrasound to externally control the release of biological substances. In the case of TriggerINK, these are growth factors and anti-inflammatories. These molecules are prepared with carrier particles that change when subject to mechanical force. For instance, the application of ultrasound causes the carrier particles to release the growth factors or anti-inflammatories deep in the tissue—at precisely the right time and location.
“Until now, one drawback with this type of activation has been the high ultrasound intensities required,” says Andreas Hermann. One of his students demonstrates the problem by putting a transparent liquid in a small tube and inserting it in a box-shaped, high-powered ultrasound device. The sound pressure causes the liquid to turn blue—during the process, however, the researchers must either wear protective earmuffs or leave the room.
Such high sound pressures are obviously unsuitable for use in practice. “But recently we’ve achieved a breakthrough,” says Andreas Hermann. “We proved that we could activate enzymes in the body also with much lower levels of sound pressure.” In their tests using a handheld ultrasound scanner, the researchers succeeded in activating the immune cells of sick mice, thus shortening their recovery phase.
There remains just one final component to complete the cartilage-healing bio-ink of the future: contracting and expanding microgel particles that mechanically stimulate the cells. These particles are produced in Laura De Laporte’s lab using a special technique to create a controlled emulsion. In tiny ducts, the liquid hydrogel forms small drops when it’s mixed with oil. Depending on duct size, flow conditions and properties of the liquid, different drop shapes result. The drops are illuminated in the duct and harden as microgel in the form given by the conditions. The aim of the researchers is to produce a whole library of such microgel shapes and to test their properties. “We don’t yet know which magnitudes are most suitable for our project,” De Laporte says.
Healing through movement
The microgels are to function like tiny little sponges in the bio-ink: infrared light impulses that penetrate deep into the tissue will cause the microgels to collapse—they wring themselves out and become smaller. This shrinking is what sets the surrounding hydrogel and the growing tissue in motion, thus accelerating the healing process.
Although regenerating cartilage with the TriggerINK method remains a long-term vision, the various subprojects are gradually forming a whole. Preliminary experiments have shown that the magnetic rods in the bio-ink influence the direction of cell growth. After the rods have been aligned in a certain direction, the cells are left to grow for several days. When observed under the microscope, it can be seen that they do indeed grow along the rods.
Teamwork and communication
It’s fair to say that the ambitious TriggerINK project is off to an excellent start. And that, explains Laura De Laporte, is also thanks to Arne Lüken, the project’s outstanding coordinator. Depending on the issue and objective, one of his many responsibilities is bringing the individual research groups and subgroups together. Something he does very well, as Laporte says, adding: “The team are passionate about the project. It has led to new collaborations within DWI and allowed the researchers to get to know each other better. That’s great for those involved, and the whole Institute benefits.”

A sophisticated plan
To stimulate rapid and targeted cell growth, the TriggerINK team are benefitting from a broad range of sophisticated, cutting-edge procedures. Their plan to stimulate cartilage growth comprises the following steps:
> Using a 3D printer, hydrogel—a gelatinous substance made of mostly water and a small amount of a bio-compatible polymer—is printed layer for layer onto the sterilised cartilage of a patient. The extremely porous hydrogel “bio-ink” forms a type of scaffold through which the cartilage tissue can regrow.
> The hydrogel is packed with particles that are import-ant for cell growth in various ways. For instance, it contains magnetic gel rods with a diameter of two to five micrometres and a length of around fifty micrometres. As long as the hydrogel scaffold remains pliable, the gel rods can be aligned by activating a weak external magnetic field. The rods control the growth direction of the cartilage cells: the cells sense the resistance from the rods and grow parallel to their alignment.
> Particles containing growth factors or anti-inflammatory substances are also integrated in the hydrogel. As a remarkable feature, ultrasound can be used to stimulate the particles into releasing the substances locally and at specific times, thereby allowing the researchers to control various actions such as the activation of cell growth.
> A final component of the hydrogel are microparticles that can be manipulated externally using light. Depending on the intensity, the particles change in size, expanding and contracting and thus setting the surrounding tissue cells in motion. Previous research indicates that such movements accelerate the healing process.
First successes
A tour of the lab at DWI shows precisely how much research and collaboration is required to make this plan a reality. Nonetheless, it’s equally clear that even after only one year, many components of the TriggerINK project are on a promising path.
For instance, Laura De Laporte’s research group has already constructed a bio-ink. “We know that cells love this hydrogel and grow well in it,” she says. In the patient, it’s vital that the polymer strands of the hydrogel combine to form a hard, scaffold-like structure, but this crosslinking process should take place only after the magnetic rods in the gel are correctly aligned. This means the process must be activated externally.
Developing such an external control system is the work of Stefan Hecht’s research group. One idea is to use chemical methods to affix certain molecules to the ends of the individual hydrogel polymer strands, thereby forming a type of protective cap that prevents crosslinking from occurring until the magnet rods are correctly aligned. Then, light is used to release the protective caps from the ends of the hydrogel strands, and the polymers are free to crosslink. One problem with this method is that the released molecules remain as a by-product in the body. “It’s difficult to predict whether and how they may react with other substances,” says Stefan Hecht.



